Has your doctor told you that you have early signs of Osteoporosis? May is National Osteoporosis Month, and women over 50 should take bone health seriously. As we age, we experience hormonal changes, particularly a decrease in estrogen levels, making it important to watch for signs of Osteoporosis over 50 years of age. In this blog, you will find some important info about Osteoporosis and 5 proven pilates strategies to crush Osteoporosis and other ideas for Osteoporosis exercises.
Osteoporosis is more common in women. It affects almost 20% (1 in 5) of women aged 50 and over and almost 5% (1 in 20) of men aged 50 and over. Many people with Osteoporosis do not know they have it until they break a bone. Screening is important to identify these people before this happens, so they can take steps to decrease the effects of Osteoporosis.
Currently, screening for Osteoporosis is recommended for women who are 65 years old or older and for women who are 50 to 64 and have certain risk factors, which include having a parent who has broken a hip.
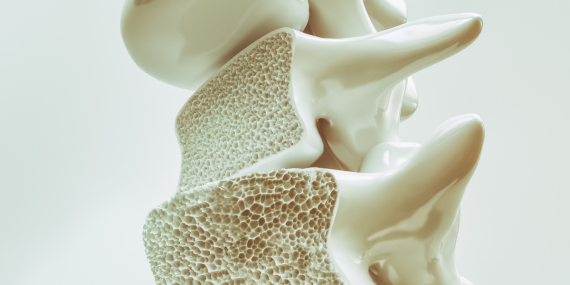
Definition of Osteoporosis
Osteoporosis is when the bones become less dense and more likely to fracture. Fractures are not uncommon as we age, but bone loss can also result in loss of height, severe back pain, and change in posture. This affects how we walk and can eventually result in permanent disability. Osteoporosis is known as the “silent killer” as it can progress undetected without any symptoms.
Risk factors for developing Osteoporosis include:
- Thinness or small frame.
- Family history of the disease.
- Being postmenopausal and particularly having had early menopause.
- Abnormal absence of menstrual periods (amenorrhea).
- Prolonged use of certain medications, such as those used to treat lupus, asthma, thyroid deficiencies, and seizures.
- Low calcium intake.
- Lack of physical activity.
- Smoking.
- Excessive alcohol intake.
3 interesting facts about Osteoporosis:
- Getting enough calcium and Vitamin D is only the first step to getting stronger bones
- Osteoporosis can go undetected for years. That’s why early detection is key.
- Osteoporosis can’t be cured but can be treated effectively!

Common Osteoporosis Symptoms
Since Osteoporosis is labeled a “silent killer”, some telltale signs might indicate that your bones are becoming brittle or showing signs of low bone density. Here are some common Osteoporosis symptoms:
- Brittle nails: Nails that easily break, split, chip, or curl around the fingertips, and dryness, discoloration, and ridges are important signs of low bone density. The most common reasons for brittle fingernails are hormonal changes and nutrition deficiencies. Women who are going through menopause have fluctuating estrogen levels.
- Receding gums: Research suggests bone loss in your jaw and mouth can be a sign of bone loss in other areas of your body. If your jawbone deteriorates, your gums will follow suit and recede.
- Weak grip strength: Grip strength may be an indicator of your overall bone density, according to a study published in Rheumatology. Female participants showed a link between grip strength and bone mineral density. Those with low grip strength have correspondingly low bone mineral density measurements in the spine and hip. The risk of vertebral fracture also increased as grip strength decreased.
How quickly does Osteoporosis progress?
Between the ages of 30 and 35, people typically start to experience bone loss at a rate of around 0.25% per year. The rate of bone loss can vary due to genetic and environmental factors.
Genetic risk factors you can’t change:
- Gender: Women are at greater risk for needed Vitamin D changes in menopause
- Age: The older you are, the greater the risk of thinning of the bones as you age.
- Body size: Small, thin-boned women are at a greater risk.
- Ethnicity: Caucasian and Asian women are at the highest risk. African American and Hispanic women have a lower risk.
- Family History: Parents with a history of fractures due to heredity.
We’ll talk about the lifestyle changes a little bit later.
Reference: 5 Ways To Prevent Osteoporosis Over 50

5 Key Reasons Why Women Over 50 Must Prioritize Bone Health for Better Osteoporosis Management
- Osteoporosis: The obvious one! Women are at a higher risk of developing Osteoporosis, a condition where the bones become weak and fragile as they age. This is especially true after menopause when estrogen levels decrease significantly. Estrogen helps maintain bone density so that this hormonal shift can lead to bone loss.
- Fractures: With reduced bone density, women over 50 are more susceptible to fractures, particularly in the hip, spine, and wrist. Fractures can lead to chronic pain, disability, and a decline in overall quality of life.
- Slower healing: As people age, their ability to heal from injuries and fractures slows down. This can further complicate fractures and increase the risk of complications, such as infections and non-union (when a broken bone fails to heal).
- Posture and balance: Poor bone health can lead to spinal deformities and a loss of height, affecting posture and balance. This increases the risk of falls and subsequent fractures.
- Independence and quality of life: Maintaining strong bones helps ensure that women can remain active and independent as they age. This is essential for overall well-being and maintaining a high quality of life.
Falls are a major concern with Osteoporosis. People with Osteoporosis are likelier to break bones, most often in the hip, forearm, wrist, and spine. While most broken bones are caused by falls, Osteoporosis can weaken bones to the point that a break can occur more easily, for example, by coughing or bumping into something.
Resources: How To Prevent and Relieve Joint Pain
Nutrition and Osteoporosis
Proper nutrition is crucial for maintaining overall health, including bone health. However, it’s important to note that diet alone may not be enough to prevent or manage conditions like Osteoporosis. Incorporating a well-rounded approach, such as Pilates and other exercises specifically tailored for Osteoporosis, can greatly benefit individuals with bone health concerns.
Some nutrition strategies to remember:
- Limit excessive sodium: Choose low-sodium options and reduce processed foods, canned goods, salty snacks, and cured meats.
- Moderate caffeine intake: High caffeine consumption may affect calcium absorption and bone loss.
- Control alcohol consumption: Stick to one drink per day for women and two drinks per day for men.
- Reduce soda intake: Limit soft drinks, especially cola, and choose healthier alternatives like water, herbal tea, or infused water.
- Be cautious with oxalate-rich foods: Those with kidney stones or specific medical conditions should watch their intake of high-oxalate foods like spinach, beet greens, rhubarb, and Swiss chard.
- Balance animal and plant-based proteins: Focus on lean protein sources like poultry, fish, beans, and lentils.
- Avoid smoking: Smoking impairs calcium absorption, and excessive alcohol intake can interfere with bone formation and increase fracture risk.

The Importance of Calcium and Vitamin D :
- Eat foods high in calcium: Calcium helps make bones strong. Include foods like milk, yogurt, cheese, kale, bok choy, broccoli, almonds, and fortified foods like orange juice, cereal, and tofu.
- Get enough Vitamin D: Vitamin D helps your body use calcium. You can get Vitamin D from sunlight, certain foods (like fatty fish, egg yolks, fortified milk, and orange juice), and supplements.
Talk to your doctor about calcium supplementation and determine your recommended intake of Vitamin D.
Resources: 6 Ways To Naturally Reduce Inflammation In The Body
Essential Osteoporosis Exercises
The best Osteoporosis exercises focus on building and maintaining bone density and improving balance and muscle strength to reduce the risk of falls and fractures.
Create a balanced workout schedule with the ideas below:
- Weight-bearing exercises: Your body works against gravity, stimulating bone formation and helping maintain bone density. Walking, jogging, hiking, dancing, climbing stairs, or jumping rope.
- Resistance training: Strength-training exercises help build muscle mass and strengthen the bones. Use free weights, resistance bands, your own body weight, or weight machines in the gym. Squats, lunges, push-ups, and upper and lower body exercises. Target all muscle groups – especially the back, to promote a strong spine.
- Balance exercises: Better balance can reduce the risk of falls, which is particularly important for Osteoporosis. Things like standing on one leg, Yoga, Thai Chi, and standing Pilates exercises.
- Flexibility exercises: Maintaining flexibility helps improve overall mobility and reduces the risk of injury. Pilates and other forms of gentle stretching.
Aim for at least 30 minutes of physical activity most days of the week. Avoid prolonged sitting and spread movements out during the day. Swimming, as good as it is for the body, does not qualify as a weight-bearing exercise.
Resources: Check out the Fearlessly Fit Over 50 Exercise Membership.
How do impact exercises affect our bodies?
Impact exercises and activities can positively and negatively affect bone and joint health. It’s essential to understand these effects and take appropriate precautions to ensure the overall well-being of your bones and joints.
Positive effects of impact exercises:
- Bone density improvement: Weight-bearing and impact exercises stimulate bone formation and help maintain bone density. Walking, jogging, dancing, or jumping can benefit bone health, particularly in preventing or managing Osteoporosis.
- Muscle strength and joint stability: Impact exercises can help improve muscle strength and joint stability, providing better support for bones and reducing the risk of injury.
Negative effects of impact exercises:
- Joint stress: High-impact exercises can place significant stress on joints, potentially causing inflammation, pain, and wear and tear. Individuals with joint conditions such as arthritis or joint injuries or who are overweight may be at a higher risk of joint issues from high-impact exercises.
- Risk of fractures: High-impact activities can increase the risk of fractures, particularly in individuals with low bone density or Osteoporosis.

Pilates Exercises for Osteoporosis
It can be a beneficial exercise option for individuals with Osteoporosis when practiced with modifications and caution. Pilates with post-menopausal women has been shown to increase bone mineral density in a study by the NIH.
These targeted exercises help to improve muscle strength, posture, balance, and flexibility, all of which are essential for reducing the risk of fractures and maintaining independence as we age.
Resource: Check out my video on how to find the Pilates posture.
Therefore, combining the right nutrition strategies with a focus on Pilates, strength, balance, and flexibility exercises can provide a comprehensive and effective approach to managing Osteoporosis and promoting optimal bone health.
The 5 Benefits of Pilates as a form of Osteoporosis Exercises
Discover the transformative power of Pilates as a form of Osteoporosis exercise as we delve into the top 5 benefits it offers for better bone health and overall well-being:
- Improved muscle strength: Pilates exercises can help increase muscle strength, particularly in the core, back, and pelvic muscles. This improved strength can provide better support for the spine and enhance overall stability.
- Better balance and coordination: Pilates exercises often emphasize balance and coordination, which can help reduce the risk of falls.
- Enhanced posture: Pilates can improve posture by strengthening the muscles responsible for maintaining proper spinal alignment. Good posture can help minimize stress on the spine and reduce the risk of vertebral fractures.
- Increased flexibility: Pilates exercises promote flexibility, improving overall mobility and decreasing the risk of injury.
- Mind-body awareness: Pilates encourages a strong mind-body connection, which can help increase body awareness and promote healthier movement patterns. Focus on slow, controlled movements when exercising.
Safe Pilates Mat Exercises For Osteoporosis
Here is a list of Pilates mat exercises specifically modified for Osteoporosis:
- The Hundred – head down
- Single Leg Circles
- Single Leg Stretch – head down
- Double Leg Stretch – head down
- Single Leg Pull – head down
- Backstroke – head down
- Criss-Cross – head down
- Swan Dive – level 1
- Single Leg Kick
- Double Leg Kick
- Shoulder Bridge
- Side Kick Series
- Hip Circle
- Swimming
- Leg Pull Front
- Leg Pull
- Side Kick Kneeling
- Push-up
Emphasize exercises that promote spinal extension, as these can help counteract the tendency for the spine to curve forward as a result of Osteoporosis.
Resources: Check out the Fasted + Fit Over 50 JumpStart
Exercises to avoid or modify:
- Avoid exercises that encourage significant spinal flexion, rolling on the back, flexion/rotation combined, extreme extension, or any exercise with a risk of falling.
- Avoid forward bending and twisting, which can put excessive pressure on the vertebrae, increasing the risk of fracture. These are Rollup, roll over, rolling like a ball, saw, corkscrew, teaser, and spine twist.
5 Proven Pilates Strategies to Crush Osteoporosis Over 50
- Choose weight-bearing exercises: Include weight-bearing Pilates exercises in your routine, such as standing exercises, to help stimulate bone growth and improve overall bone density.
- Prioritize posture and alignment: Focus on proper posture and alignment during your Pilates practice to help reduce the risk of fractures, maintain spinal health, and minimize the impact of Osteoporosis on your daily life.
- Strengthen your core: Incorporate core-strengthening exercises in your Pilates sessions to support your spine, improve stability, and enhance overall balance, reducing the risk of falls and fractures.
- Proper technique: Ensure that you use proper form and technique during impact exercises to minimize stress on joints and reduce the risk of injury. Work with a knowledgeable Pilates instructor who can help modify exercises to suit your needs and limitations.
- Consistency is key: Practice Pilates regularly to experience its full benefits on bone health, strength, and balance. Aim for at least 2-3 sessions per week, gradually increasing the intensity and duration as your body adapts and grows stronger.
Embracing the benefits of improved coordination, core and hip strength, optimal posture, and balance will help prevent falls and prepare your body for activities involving higher loads, such as weight training. Individuals with Osteoporosis can enjoy a healthy, strong, and fracture-free life by integrating modified Pilates exercises. Gradually increase the intensity, duration, and frequency so your bones can adapt safely.
Cross-training is a critical aspect of creating strong bones and better health. Choose low-impact to moderate-impact exercises you love, add some Pilates and strength training sessions, and sprinkle in some stretching.
Resources: Pilates Over 50 – Is It Too Late To Start Now?
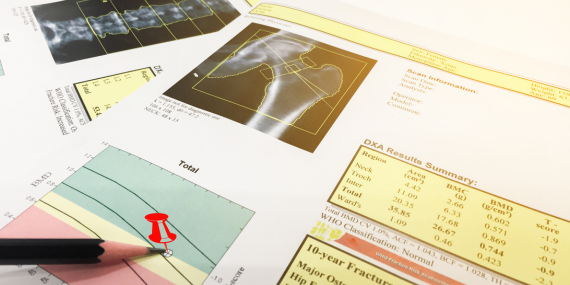
How do you check for bone density?
A DEXA scan is the most common way to measure bone density. DEXA stands for dual-energy X-ray absorptiometry.
However, your healthcare provider may order more tests to confirm a diagnosis or determine whether bone loss treatment works. These include a calcium blood test, a Vitamin D test, and tests for certain hormones
In conclusion, monitoring your bone health, being mindful of your diet, and incorporating Pilates for Osteoporosis and other Osteoporosis exercises into your lifestyle can significantly contribute to optimal bone health.
Thank you for this comprehensive information. Bone health and bone loss are complex events and knowledge is key in fostering the best outcome! Such a valuable resource!!
Thank you, Barbie, this means a lot to me.
Very well researched-I have bookmarked this post for future reference. Thank you!!
I appreciate you. Thank you.
Such very important information. I wish I knew this decades ago as I have degenerative arthritis and have had two hips replaced. Thank you for sharing im sure this will enlighten others to take notice and practice ways to improve our bone density.
Thank you Nancy, for sharing this personal information with me and please pass on the blog to others.
An excellent, detailed post! I have been worried about bone health especially since I turned fifty. I’ve never enjoyed drinking milk so I’ve been trying to add more fortified plant based beverages to my daily diet (as well as eating greens and other sources of calcium). I’ve bookmarked your post for reference so that I can start incorporating some of the exercisesyou recommend, too. Thank you! Xo Nipa
Nipa,this means a lot to me and bone health is something so many women don’t give a thought until a DEXA scan is the wake up call. Please share with anyone you think might benefit from this. Thank you 🙂
*exercises not excel uses – I didn’t catch the autocorrect before I posted my comment!
fixed it 🙂
Comments are closed.